APOE4, the Gut Microbiome, and the Missing Piece in Lipid Transport
What a New Study Really Tells Us — and What We Can Do About It
Much of the conversation around APOE4 has focused on what goes wrong later - amyloid, plaques, cognitive decline. Far less attention has been paid to the upstream biology that shapes risk decades earlier. One important upstream systems is the gut microbiome, which quietly influences inflammation, metabolic signaling, and lipid handling long before any symptoms appear. Emerging research suggests that for APOE4 carriers, the gut may act less as a bystander and more as a modifier of long-term brain resilience.
A recently published paper adds to that picture by examining how the gut microbiome differs between APOE4 carriers and non-carriers in cognitively healthy older adults. The differences are subtle, but they matter because they point to low-risk, high-upside ways APOE4 carriers can reduce inflammatory pressure and support the systems that APOE4 strains over decades.
What the study looked at
Researchers analyzed stool samples from 114 cognitively healthy adults (average age ~77) and compared APOE4 carriers with non-carriers. Importantly, these were not people with Alzheimer’s. These were older adults aging normally.
That matters, because it shifts the question from disease to risk biology.
The key finding
APOE4 carriers did not have worse overall microbiome “richness” (how many species live in the gut). But they did show differences in microbial composition compared to non-carriers.
In other words:
It’s not about how many microbes you have
It’s about which ones dominate and what they do
Notably, the study highlighted species differences tied to short-chain fatty acid (SCFA) pathways, including butyrate—a compound associated with:
Gut barrier integrity
Immune regulation
Microglial balance
Neuroinflammation control
This aligns with the broader pattern across APOE–microbiome research: the most consistent signal isn’t one “magic bacteria,” it’s function - inflammation tone, barrier integrity, and microbial metabolites like SCFAs.
Where lipid transport fits in
APOE4’s core problem in the brain isn’t “cholesterol is bad.” It’s that lipids and cholesterol aren’t moved around as efficiently, especially for repair and maintenance.
Think of ApoE as a delivery system: neurons and synapses rely on lipid transport for membrane repair, signaling, and resilience. APOE4 tends to be a less efficient delivery version, and it’s more vulnerable when inflammation is high.
This is where the gut matters.
The gut can worsen or ease APOE4’s lipid-transport burden in 3 practical ways:
1) Inflammation is a headwind for lipid handling
A disturbed microbiome can increase inflammatory signaling through the immune system. Chronic, low-grade inflammation makes the brain’s support cells (astrocytes and microglia) less “repair oriented,” which is the exact environment where APOE4 struggles most.
2) The gut helps regulate bile signaling and fat processing
Our gut microbes interact with bile acids (which start as cholesterol). Those bile-related signals influence metabolic tone and inflammatory set points. When that system is off, lipid handling tends to get messier, systemically and in the brain.
3) SCFAs help keep the barrier intact
Butyrate-supportive ecosystems are linked with healthier gut barrier function and calmer immune signaling. A better barrier typically means fewer inflammatory triggers leaking into circulation - again lowering the pressure on APOE4’s already-fragile risk biology.
Bottom line: Supporting gut function can lower the inflammatory “noise” that makes APOE4 lipid transport inefficiency more damaging over time.
What we can reasonably extrapolate (and what we can’t)
Taken in context with other studies in humans and APOE-targeted replacement mice, this paper supports a larger pattern:
APOE4 is associated with a pro-inflammatory bias
The gut microbiome appears to be one contributor to that bias
SCFA-supportive ecosystems may be less supported in APOE4 carriers
That may amplify vulnerability over decades
Crucially, the microbiome is modifiable - unlike our genes.
Where TUDCA fits into the APOE4 gut-lipid picture
An often-overlooked piece of gut health is bile flow and bile signaling, which sits at the intersection of cholesterol metabolism, microbial ecology, and inflammation. TUDCA (tauroursodeoxycholic acid) supports healthy bile composition and flow, helping the body properly emulsify fats and recycle cholesterol-derived bile acids. This matters for APOE4 because bile acids are not just digestive detergents - they are signaling molecules that influence metabolic tone, inflammatory pathways, and gut microbial balance. When bile flow is sluggish or bile signaling is disrupted, downstream effects can include dysbiosis, impaired lipid handling, and increased inflammatory burden - all areas where APOE4 carriers are more vulnerable. By supporting bile physiology, TUDCA may indirectly reduce stress on lipid transport systems and help create a gut environment that is more compatible with long-term metabolic and brain resilience.
An APOE4-focused action plan (low risk, high upside)
Rather than chasing individual bacteria, the goal is to shift gut function, not taxonomy.
Start with data
If you’ve never done a microbiome stool test, this is an excellent place to start. Many of us have taken antibiotics at some point, and those are well known to disrupt beneficial gut bacteria. A microbiome test removes the guesswork and allows you to build a targeted, informed action plan.
Looking back at my own results, I learned I was low in key strains such as Akkermansia and L. reuteri, which helped me adapt my strategy with precision. Tiny Health, a leader in microbiome testing, offers a simple at-home test with clear, actionable insights. Use code APOE44 to save $20 on your test.
1) Support short-chain fatty acid production
SCFAs, especially butyrate, are one of the most consistent protective signals in gut–brain research.
Practical ways to do this:
Gradually increase fermentable fiber diversity, not just quantity
Examples: overnight oats or barley (beta-glucans), legumes if tolerated, psyllium, PHGG, inulin, cooked-and-cooled starches
Go slow—tolerance matters more than perfection
2) Use fermented foods strategically
Small, regular amounts can help reshape microbial signaling:
Kefir, yogurt, sauerkraut, kimchi, fermented vegetables
Start with tablespoons, not bowls
Back off if histamine or GI symptoms flare
3) Think “polyphenols feed microbes”
Polyphenols can shift microbial function even when species changes are subtle:
Berries, cocoa, green tea, herbs, spices, pomegranate
4) Protect the gut barrier
A stressed gut barrier can amplify systemic and neuroinflammation.
Minimize ultra-processed foods (and pay attention to emulsifiers if sensitive)
Be mindful with alcohol
Prioritize sleep and circadian consistency
Ensure adequate omega-3 intake
5) Be intentional after antibiotics or illness
Treat recovery periods as “rebuild windows”:
Re-emphasize fibers, fermented foods, and polyphenols
Don’t assume you “bounce back” automatically
What I personally do to support gut health
After years reading about the gut–brain connection (and taking a microbiome test), I’ve landed on an approach that’s simple, consistent, and physiologically sensible rather than extreme.
My non-negotiable foundation is real food - focused on supporting the gut lining and microbial diversity:
Homemade kefir (which I tolerate well and make regularly)
Non-pasteurized sauerkraut for natural lactobacilli and fermentation byproducts
A diet that excludes ultra-processed foods, sugar, simple carbs, and seed oils
On top of that base, I use a few targeted supports:
Butyrate (mornings, empty stomach) to support gut barrier integrity
TUDCA (with breakfast) to support bile flow and fat digestion—an often-overlooked part of gut health
Akkermansia (Pendulum) and L. reuteri as targeted supports rather than “dozens of strains” … both also taken on an empty stomach.
Where saffron fits in (and why I’ll continue using it)
One addition that’s been surprisingly impactful for me is saffron. (wrote about its potent effects in a previous post.)
From a metabolic perspective, saffron supports:
insulin sensitivity
reduced inflammatory signaling that interferes with glucose regulation
healthier gut–liver–bile signaling (which affects metabolic control)
The bigger picture
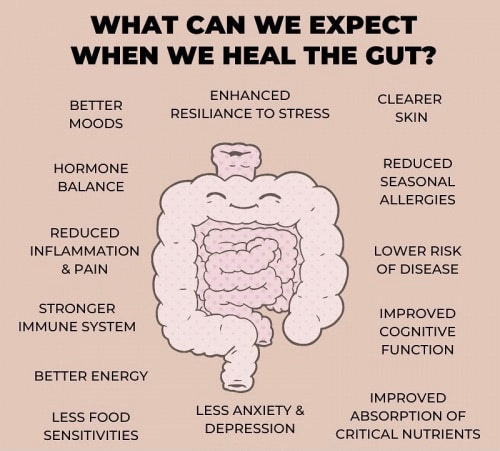
For APOE4 carriers, gut health isn’t just digestive health. It’s brain health.
Genes load the gun, but environment pulls the trigger - and the microbiome is one of the most powerful, most modifiable environmental levers we have.
And unlike many interventions in Alzheimer’s prevention, improving gut ecology is:
low risk
multi-system beneficial
compatible with almost every other strategy
This isn’t about doing everything.
It’s about doing enough of the right things, consistently - and paying attention to how our body responds.
References:
https://pmc.ncbi.nlm.nih.gov/articles/PMC12737834/
https://pmc.ncbi.nlm.nih.gov/articles/PMC6593891/
https://pmc.ncbi.nlm.nih.gov/articles/PMC12081816/
https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2021.619051/
https://www.sciencedirect.com/science/article/pii/S2589004224015736

Another great article with specific actions I can start today! Thank you!!
Thank you for the post!🙌